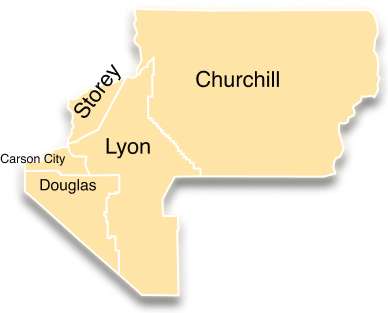
The Northern Behavioral Health Region
The Northern Region consists of Carson City, Churchill, Douglas, Lyon, and Storey Counties, stretching across 8,049 square miles in northwestern Nevada. The total population of the Northern Region, close to reaching 200,000, is largely rural in nature, with several city hubs including Carson City, Minden, Gardnerville, Dayton, Fallon, and Fernley.
Northern Regional Behavioral Health Resource Guide (2023-2024) Online Version
Members serving on the Northern Regional Behavioral Health Policy Board are community leaders, law enforcement, healthcare and treatment providers, family and peer advocates, and more. They bring diverse perspectives to the Board and are passionate about collaborating to improve the behavioral health system in the Northern Region. Collaboration facilitated by the Northern Regional Behavioral Health Policy Board and associated county behavioral health taskforces, has enabled stakeholders to develop a shared understanding of the behavioral health issues facing the region. This has allowed the Northern Board to achieve substantial progress on its goals by working with local, regional, and state partners to identify and align priorities and solutions whenever possible. Through ongoing discussion, the Northern Regional Behavioral Health Policy Board members, shown below, identified the Northern Region’s gaps, needs, priorities, and recommendations for this annual report.
Members:
Chair: Shayla Holmes, Executive Director of Lyon County Health and Human Services
Vice Chair: Laura Yanez, Executive Director, NAMI Western Nevada
Dr. Robin Titus, Senator, Legislator
Dr. Ali Banister, PhD, Juvenile Probation Chief – First Judicial District
Nicki Aaker, RN, Director, Carson City Health and Human Services
Erik Schoen, Executive Director, Community Chest
Ken Furlong, Sheriff, Carson City
- Sandy Wartgow, Carson City Fire Department
Lana Robards, Director, New Frontier Treatment Center, Fallon, Nevada
- Daria Singer, Executive Director, Partnership Douglas County
Alana Rogne, Medical Director, Rural Nevada Counseling
- Erin Dudley, Behavioral Health Manager, Carson Valley Health
- Lori Follett, Social Services Chief II, Department Health Human Services / Health Care Financing and Policy / Behavioral Health Benefits Coverage Team
- Continue to obtain sustainable funding for current crisis stabilization and jail diversion programs (MOST, FASTT, CIT, and Carson Tahoe Mallory Crisis Center)
- Increase behavioral health workforce with the capability to treat all ages across the continuum
- Increase access to treatment at all levels of care (health and behavioral health)
- Increase access to affordable and supported housing
- Develop services to support continuity of care (e.g. continuation of medication/ service connection with community health worker and peers)
While the Northern Region does not have the data to quantify the issues below, stakeholders throughout the region have identified the following trends from various perspectives in the community:
- Increased crisis in older adults leading to increased need for crisis response and hospitalizations
- An increase in youth experiencing mental health crises, suicidal thoughts, and behaviors
- Problems for youth and families accessing both outpatient and inpatient treatment
- An increase in adults attempting to access treatment
- Increased need for food and shelter assistance
- Behavioral health needs caused by COVID-induced risk factors (this is prominent across disciplines)
- Increase in emergency calls from seniors struggling with dementia
2025 Northern Board Legislation: AB 60
AN ACT relating to behavioral health; requiring the certification of a natural person who holds himself or herself out as a certified prevention specialist; prohibiting a minor from providing or supervising the provision of peer recovery support services in most circumstances; authorizing certain minors to serve as peer recovery support specialist interns; authorizing the imposition of civil penalties for certain violations; prohibiting the employment or retention as an independent contractor of a natural person to serve as a certified prevention specialist in a position where the natural person has regular and substantial contact with minors if the natural person has been found to have engaged in certain conduct; requiring a certified prevention specialist to report certain information; requiring a substance use disorder prevention coalition to employ or enter into contracts with certified prevention specialists for certain purposes; and providing other matters properly relating thereto.
Ongoing Regional Behavioral Health Planning Efforts
County Behavioral Health Task Force Strategic Planning
Each county in the region has developed behavioral health task forces and community meetings to respond to their community’s health and behavioral health needs. For some counties, this strategic planning process has occurred over multiple workshops and meetings that have focused on general strategic planning for behavioral health and specific issues such as the Stepping Up Initiative. Priorities identified in planning efforts have been incorporated into “living” strategic planning documents that are updated as new issues arise or when progress is made. These behavioral health task forces and strategic planning sessions receive input from diverse community stakeholder groups, including EMS/ Fire, law enforcement, county officials, social services, behavioral health treatment providers, hospitals, and peer and family advocates. These county-based strategic planning efforts provided a vital source of information for the Northern Regional Behavioral Health Policy Board strategic plan.
Regional Crisis Now Planning
In early 2020, the Northern Board initiated regional efforts to conduct a gap and needs analysis to inform the DPBH’s Crisis Now Initiative. More information on the Crisis Now initiative can be found here: https://socialent.com/2020/06/nevada-crisis-response-system-virtual-summit/. Through this process, stakeholders identified several resources already in place to support Crisis Now, including the Mobile Outreach Safety Teams, Crisis Intervention Training, and Mallory Crisis Center. In addition, the region also identified the following needs to develop a cohesive Crisis Now system in the region:
- 24/7 mobile crisis response: The region’s MOST teams are currently strained by community needs and are not 24/7. MOST is important in connecting with individuals who lack insight into their mental illness or who are at risk of violence. In addition to the MOST teams, the region hopes to develop centralized 24/7 mobile crisis teams staffed by clinicians and peers to respond to voluntary and non-violent individuals. The Northern Region’s stakeholders believe that having both MOST and mobile crisis teams is an adaption to the Crisis Now model that will meet the unique needs of Nevada.
- Crisis call coordination: While the Northern region has access to many hotlines, it needs to be connected with a central crisis call line providing “care traffic control.” Currently, Crisis Support Services of Nevada (CSSN) is intended to provide that function for the state; however, MOUs and shared processes are still needed between the region’s local providers and CSSN.
- Crisis Stabilization Unit: The region is fortunate to have the Mallory Crisis Center, which has successfully provided crisis stabilization for the region and rural counties for several years now. The Northern Board has prioritized the need for the state to develop a sustainable funding model for Mallory to ensure long-term success.
- Rural crisis stabilization access points: Due to the Northern Region’s geographic area, stakeholders identified the need for crisis stabilization access points in its more rural areas. The region’s CCBHCs may be able to provide this function, but at this time, none have a formal crisis stabilization area with 24/7 support needed for law enforcement drop-off. In addition, there is an opportunity for our rural critical access hospitals to develop scale-down crisis stabilization services.
The process of building and designing the Nevada 988 Crisis Response System is still ongoing, but the marathon is being run, and we are approaching mile markers every month. As the state works on building its three-pronged crisis response system to fidelity, it has recently solidified Nevada’s new 988 provider. This step was a huge hurdle, but Nevada now has a 988 provider Carelon helping move us move in the right direction for crisis response. Forward movement is being recognized weekly. More to come as Nevada moves forward with 988 and its implementation.
We respectfully present the following list of recommendations for the Northern Regional Behavioral Health Policy Board. These recommendations are listed in order of board member ranking:
1. Obtain sustainable funding for crisis stabilization and criminal justice diversion initiatives and programs including: MOST, FASTT, CIT and Mallory Crisis Center.
As noted above, these crisis stabilization programs have significantly assisted the region in responding to individuals in behavioral health crisis. The Board recommends obtaining long term funding for these programs to ensure that the progress gained in the region would not be lost.
2. Support continued funding for Regional Behavioral Health Coordinator position.
Our region continues to advocate for a sustainable funding stream to maintain the regional behavioral health coordinator position. We deeply value our coordinator with her longstanding commitment to the position and experience. The board recommends that the state sustain current funding levels to attract qualified candidates for this essential position. In addition, the coordinator position is tasked with coordinating the region’s initiatives, providing technical assistance, and administrative support to the board. Ideally, the board could use more staff to support administrative activities, development of data reporting, and initiatives moving forward. This neutral position, funded by the state, but housed in a community organization, facilitates collaboration between local, regional, and state stakeholders that reduces silos, fosters honest discussion about gaps and needs, and develops innovative solutions to shared problems.
3. Support the regional implementation of the Crisis Now model, supporting efforts that respect community informed solutions in addressing local and regional gaps, challenges, and existing resources.
Like the other behavioral health regions in the state, stakeholders in the Northern Region see real value in developing an alternative behavioral health crisis response system through the Crisis Now Model. As discussed above, our region has made significant progress in developing that model through our MOST co-responder teams and the Mallory Crisis Center. The board recommends that the state support the region in developing the Crisis Now model with adaptations that meet the unique needs of our region which include:
- Development of Crisis Now using locally based providers and solutions when possible.
- Access to both in-person mobile crisis response and county-based co-responder teams. Both programs respond to different populations. The mobile crisis teams respond to individuals who are voluntarily connecting with services, while the co-responder teams are able to use wellness checks to build rapport with individuals who lack insight into their illness or may not be motivated by treatment.
- Development of scaled down “living room” model crisis access points to support individuals in crisis and assess their needed level of care.
- Establish a strong coordinated relationship between state run services such as Crisis Support Services of Nevada and community owned crisis response programs and providers.
4. Increase workforce: Increasing recruitment and retention of psychiatrists, behavioral health clinicians, substance use treatment professionals, and/or behavioral health professionals with the capability to treat youth.
As discussed above, the Northern Region struggles to attract and retain a skilled workforce to provide quality behavioral health services. In addition, there is a dearth of mental health professionals who can treat youth. While the board does not have an identified solution, the board recommends the state explore mechanisms for recruitment and retention of workforce including licensing, reimbursement, and increasing local opportunities for education.
5. Increase access to residential treatment and housing: In particular, inpatient/ residential treatment and housing, and transition support to reenter community.
Stakeholders in the region continually report that there are not enough inpatient and residential behavioral health beds to care for the population. In addition, they see a gap in transitional housing and support for those reentering the community after treatment. The board recommends the state prioritize this critical issue in its policy development and planning.
6. Increase options for supportive housing.
As noted above, stakeholders in the Northern Region have reported a lack of group homes and long-term care to support individuals in chronic sub-acute crisis. Due to lack of housing, these individuals are unable to be discharged from hospitals for long periods of time or live homeless in the streets interacting with law enforcement and impacting our emergency services system. The Northern Board does not know enough about this complex issue to provide specific solutions but seeks the state’s support in identifying resources and technical assistance to progress on this issue.
7. Develop services to support continuity of care (e.g. continuation of medication/ service connection with community health worker).
As noted above, providing funding for services to support continuity of care could address the clinical workforce gaps and allow for community-based services. Several members of our Regional Behavioral Health Policy Board are interested in exploring mechanisms that support community health workers, as it is believed that these can provide community-based support and fill some of the gaps created by the lack of clinical workforce.
8. Support efforts to increase use of telehealth for behavioral health services to reach isolated populations such as rural communities and older adults.
In response to the ongoing issues with lack of behavioral health workforce, timely access to various levels of care, and the increased risk of isolation in rural communities, the Board is motivated to explore opportunities and solutions to implement and expand the use of telehealth for behavioral health services where appropriate. The Board recommends the state sustain the expanded use of telehealth that was initiated by the COVID- 19 response. This includes the use of telephones for behavioral health where videoconferencing capabilities are inaccessible. This is important as many rural counties struggle with connectivity issues and the board has heard stories of individuals experiencing challenges in affording or operating smart phones or other videoconferencing technology.
9. Develop initiatives to support regional behavioral health authorities for formalizing behavioral health infrastructure in the region, improve advocacy and collaboration with the state, and develop cost sharing among counties for behavioral health resource use.
Since the Northern Region started meeting as a coalition in 2013, stakeholders have experienced issues in applying for grants and receiving funding without a central regional authority. In addition, other states have used regional authorities to manage data and funding to respond to the unique needs of the region. The Board recommends that the State provide technical assistance in conducting a feasibility assessment.
10. Support development of behavioral health emergency response through regional and state collaborative efforts on initiatives such as PsyStart, Psychological First Aid, and Behavioral Health Disaster training for first responders.
Through multiple stakeholder workgroups and input from the Northern Regional Behavioral Health Policy Board, the Northern Region has developed a draft Northern Regional Behavioral Health Emergency Operations Plan. This plan will assist stakeholders in responding to the behavioral health needs of the community and first responders during a disaster. The Board recommends that the state provide resources and training to make this plan operational.
11. Develop increased support for older adults to maintain stability in their living environment.
Older adults in the Northern Region have experienced increased stress and isolation during COVID-19. Many of the supports and services they received in-person prior to the pandemic, such as Senior Services lunches and activities, and in-person support services were scaled down or temporarily closed, leading seniors to experience increased loneliness and less support. Community stakeholders are seeing increasing numbers of older adults experiencing crisis and need for hospitalization. The Board recommends that the state explore additional community level services be put in place to support seniors in their environments.
12. Support initiatives to increase cultural awareness and provide behavioral health services to minority populations including LGBTQA+.
The Board seeks to advance health equity in behavioral health care in our region where everyone has a fair and just opportunity to be as healthy as possible. This includes advocating for funding education on culturally competent care, which can be defined as the ability of providers and organizations to effectively deliver and promote health care services that meet the social, cultural, and linguistic needs of patients. Some examples include: educating medical professionals about healthcare challenges specific to LGBTQA+ individuals, advocating for workforce development policies that increase the number of bilingual providers in our state, working with healthcare providers and organizations to deliver unconscious bias training into the workplace, advocating for robust data collection that will help us to identify gaps in services that disproportionately impact minority populations, and developing best-practice guidelines that help behavioral healthcare providers and organizations develop a provider community that reflects the community it serves.
Advancing health equity also requires collaboration with, and support of, community partners who are removing barriers to care including food insecurity, discrimination of all kinds, and housing insecurity, to name a few. Additionally, we seek to foster collaboration and partnership with community organizations and entities that serve minority populations to learn how best to support their work, better understand the needs of the diverse populations in our region, and recruit individuals with diverse experiences and perspectives to boards such as this one.
The 2021 Nevada Bureau of Health and Wellness Epidemiological Profile for the Northern Region reported the following trends:
- A significant increase in the percentage of Northern Region residents who reported 10 or more days of poor mental health, a significant increase from 16.4% in 2018 to 26.9% in 2019.
- Anxiety has been the leading mental health-related diagnosis since 2010 in emergency department (ED) encounters. Anxiety-related encounters increased significantly from 2010 to 2019 in both counts and rates. However, ED encounters for depression have decreased from 2016.
- Depression is the leading diagnosis for inpatient admissions.
- The age-adjusted suicide rate for 2019 in Northern Region was 29.6 per 100,000 population, and there were 59 suicides in the region 2019.
- ED visits for marijuana, opioids, and heroin, increased from 2018 to 2019.
- There was an increase in drug related deaths in the region from 2018 to 2019.
More information can be found in the profile here:
Carson City
Churchill County
Douglas County
Lyon / Storey Counties
Northern Regional Behavioral Health Resource Guide (2023-2024) – Online Version
AATOD- American Association for the Treatment of Opioid Dependence
CDC: Training/Overdose Prevention Educationhttps://www.cdc.gov/overdose-prevention/communication-resources/resource-hub.html
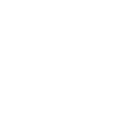
Click to select Behavioral Health Region
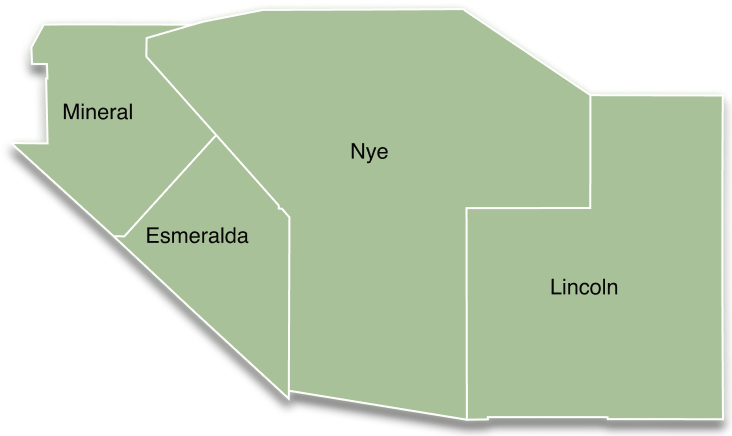
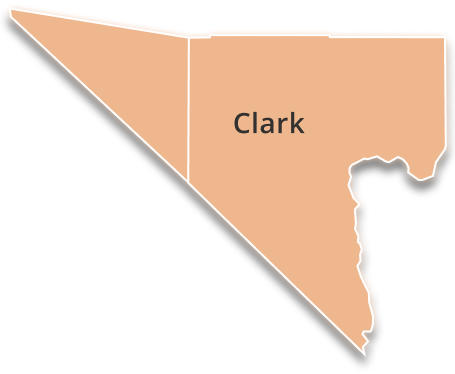
Health Region
Health Region
Health Region
Health Region
Health Region
july, 2025
News & Announcements
Publications and Reports
| Type | Group | Name | Region | Date | Download |
|---|---|---|---|---|---|
| Board Meeting, Meeting Minutes | Northern Region Behavioral Health Policy Board April 2025 Meeting Minutes | Nevada Statewide, Northern | 06/06/2025 | Preview Download | |
| Board Meeting, Meeting Minutes | Northern Regional Behavioral Health Policy Board March 2025 Meeting Minutes | Nevada Statewide, Northern | 06/06/2025 | Preview Download | |
| Resources | Peers Together Impact Report – May 2025 | Nevada Statewide, Northern, Southern | 06/02/2025 | Preview Download | |
| Board Meeting, Meeting Minutes | Northern Regional Behavioral Health Policy Board Meeting Minutes February 2025 | Nevada Statewide, Northern | 06/01/2025 | Preview Download | |
| Report Uploads | BeHereNV Annual Report – 2024 | Nevada Statewide, Northern, Southern | 05/30/2025 | Preview Download | |
| Board Meeting | Northern Regional Behavioral Health Policy Board – June 5th, 2025 Agenda | Nevada Statewide, Northern | 05/22/2025 | Preview Download | |
| Research | Four decades of overdose prevention centres: lessons for the future from a realist review | Nevada Statewide, Northern, Southern | 05/21/2025 | Preview Download |